Knee Surgery Types: A Comprehensive Guide to Procedures & Recovery
Over 1.3 million knee surgeries are performed annually in the U.S., with global numbers surpassing 4 million, reflecting the growing burden of arthritis, sports injuries, and age-related joint degeneration. By 2025, advancements in robotics, biologics, and precision medicine have transformed knee surgery into a highly personalized field. This guide not only explores surgical options but also emphasizes the importance of patient education in navigating recovery timelines, financial planning, and lifestyle adjustments. Whether you’re a weekend warrior or managing osteoarthritis, understanding these procedures empowers you to reclaim mobility and improve quality of life.
1. What is Knee Surgery?
Knee surgery refers to a spectrum of procedures aimed at repairing damaged structures, restoring function, and alleviating pain in the knee joint. It is typically considered when conservative treatments—such as medications, injections, or physical therapy—fail to provide sustained relief.
In-Depth Knee Anatomy
The knee is a complex hinge joint involving:
- Bones: Femur (thigh bone), tibia (shin bone), and patella (kneecap).
- Cartilage: The menisci (C-shaped shock absorbers) and articular cartilage (smooth tissue covering bone ends).
- Ligaments: ACL (anterior cruciate), PCL (posterior cruciate), MCL (medial collateral), and LCL (lateral collateral), which stabilize the joint.
- Tendons: Connect muscles to bones, such as the quadriceps and patellar tendons.
Common Conditions Requiring Surgery
- Osteoarthritis (OA): Degeneration of articular cartilage, leading to bone-on-bone friction.
- Rheumatoid Arthritis (RA): Autoimmune inflammation eroding joint lining.
- Traumatic Injuries: ACL tears (common in soccer/basketball), meniscus tears, and patellar dislocations.
Why Surgery Matters
Left untreated, severe knee damage can result in chronic pain, muscle atrophy, and permanent mobility loss. For example, untreated ACL tears increase the risk of early-onset osteoarthritis by 50%, according to a 2024 American Journal of Sports Medicine study.

2. When is Knee Surgery Needed?
Surgery becomes necessary when symptoms interfere with daily life or pose long-term health risks.
Red Flags Indicating Surgery
- Persistent Pain: Pain that disrupts sleep or persists despite rest, ice, and NSAIDs.
- Mechanical Symptoms: Locking, clicking, or inability to fully extend the knee, often due to meniscus tears.
- Instability: Frequent falls or “giving way” during routine activities like climbing stairs.
- Progressive Deformity: Bowlegged (varus) or knock-kneed (valgus) alignment worsening over time.
High-Risk Populations
- Athletes: ACL tears account for 40% of sports-related knee injuries.
- Seniors: 60% of adults over 65 show radiographic signs of knee OA.
- Obese Individuals: Each pound of body weight adds 4 pounds of pressure on the knee during walking.
Case Study: A 50-year-old marathon runner with a complex meniscus tear underwent arthroscopic repair, avoiding a meniscectomy and preserving long-term joint health.
3. Types of Knee Surgery
A. Knee Replacement Surgery
Total Knee Replacement (TKR)
- Procedure: Surgeons remove damaged bone and cartilage, replacing them with metal alloy and medical-grade plastic components.
- Candidates: Patients with advanced OA affecting all three knee compartments.
- Innovations: Cementless implants with porous coatings that encourage bone growth (10% longer lifespan than traditional models).
Partial Knee Replacement (PKR)
- Procedure: Only the damaged compartment (medial, lateral, or patellofemoral) is replaced.
- Benefits: Faster recovery (4–6 weeks vs. 12 weeks for TKR) and better retention of natural kinematics.
- Limitations: Not suitable for inflammatory arthritis or widespread damage.
Revision Knee Surgery
- Causes for Revision: Infection, implant loosening, or polyethylene wear.
- Complexity: Requires specialized surgeons due to bone loss and scar tissue.
Recovery Insights:
- Weeks 1–2: Focus on knee pain management and gentle range-of-motion exercises.
- Weeks 3–6: Gradual introduction of weight-bearing and strength training.
- Long-Term: 95% of TKRs last 15+ years, per 2025 data from the American Academy of Orthopaedic Surgeons (AAOS).

B. Arthroscopic Knee Surgery
Procedure Breakdown
- Step 1: Two small incisions are made for the arthroscope (camera) and surgical tools.
- Step 2: Saline solution inflates the joint for better visualization.
- Step 3: Surgeons repair tears, remove debris, or smooth cartilage.
Common Applications
- Meniscus Repair: Peripheral tears with adequate blood supply are stitched, while complex tears may require partial removal.
- Loose Body Removal: Cartilage or bone fragments causing locking are extracted.
- Synovectomy: Inflamed synovial tissue is excised in rheumatoid arthritis patients.
Recovery Timeline:
- Day 1: Weight-bearing as tolerated with crutches.
- Week 2: Return to desk work; avoid squatting or pivoting.
- Month 2: Resume low-impact sports like swimming.
C. Knee Ligament Surgery
ACL Reconstruction
- Graft Options: Patellar tendon (gold standard), hamstring tendon, or cadaver tissue.
- Innovations: Anatomic ACL reconstruction improves graft placement, reducing re-tear rates by 20%.
PCL/MCL/LCL Repair
- PCL: Often treated non-surgically unless combined with other injuries.
- MCL/LCL: Grade III tears (complete ruptures) may require surgical reattachment.
Rehabilitation Focus:
- Phase 1 (0–6 weeks): Restore full extension, reduce swelling.
- Phase 2 (6–12 weeks): Strengthen hamstrings and quadriceps.
- Phase 3 (3–6 months): Sport-specific drills and agility training.
D. Meniscus Surgery
Meniscus Repair vs. Meniscectomy
- Repair: Ideal for red-red or red-white zone tears; 75% success rate if vascularized.
- Meniscectomy: Partial removal for complex tears; increases OA risk by 14% over 10 years.
Emerging Techniques:
- Meniscal Scaffolds: Collagen implants stimulate new tissue growth in irreparable tears.
- Allograft Transplantation: Donor meniscus grafts for young patients with extensive damage.

E. Knee Osteotomy
High Tibial Osteotomy (HTO)
- Procedure: A wedge of bone is removed from the tibia to shift weight to the healthier compartment.
- Candidates: Active patients under 60 with early-stage OA and varus deformity.
Distal Femoral Osteotomy (DFO)
- Used For: Valgus (knock-knee) alignment correction.
Long-Term Outcomes: 80% of patients delay knee replacement by 10+ years.
F. Knee Cartilage Repair
Microfracture Surgery
- Process: Tiny holes are drilled into the bone to release marrow cells, forming fibrocartilage.
- Limitations: Fibrocartilage is less durable than hyaline cartilage.
Autologous Chondrocyte Implantation (ACI)
- Step 1: Healthy cartilage cells are harvested and cultured in a lab.
- Step 2: Cells are implanted into the defect during a second surgery.
- Success Rate: 85% at 5 years for focal defects <4 cm².
G. Emerging Techniques
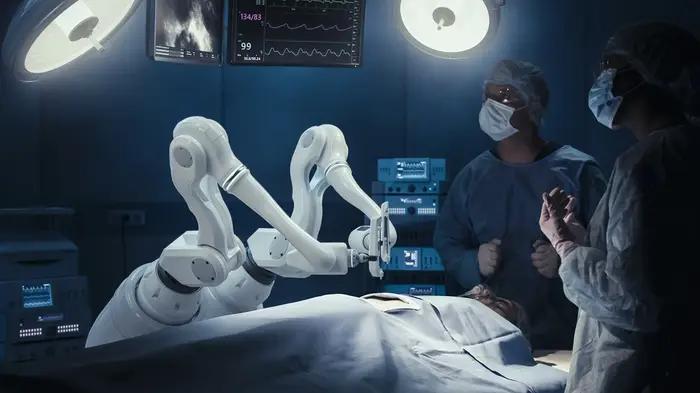
Robotic-Assisted Surgery
- Systems: MAKO, ROSA, and NAVIO robots enhance implant alignment accuracy.
- Benefits: Reduces outliers in implant positioning by 70%, lowering revision risks.
Biologic Therapies
- Stem Cell Therapy: Mesenchymal stem cells injected into the joint to modulate inflammation.
- PRP Injections: Platelet-rich plasma promotes healing in early OA (40% pain reduction in 2025 trials).
4. Preparing for Knee Surgery
Pre-Operative Checklist
- Medical Evaluation: Assess heart health, diabetes control, and infection risks.
- Imaging: 3D MRI or CT scans for surgical planning.
- Prehabilitation: 4–6 weeks of quadriceps strengthening and balance exercises.
Dietary Adjustments:
- Increase protein intake (1.2–1.5g/kg body weight) to aid healing.
- Avoid alcohol and NSAIDs 2 weeks pre-surgery to reduce bleeding risks.
5. Risks vs. Benefits
Expanded Risks
- Nerve Damage: Rare (<1%) but may cause numbness or weakness.
- Anesthesia Complications: Higher risk in patients with sleep apnea or heart disease.
- Chronic Pain: 10–15% of TKR patients report residual discomfort.
Enhanced Benefits
- Quality of Life: 90% of patients report improved mobility and pain relief.
- Economic Impact: Return-to-work rates rise by 65% post-surgery.
6. Recovery Timeline & Tips
Phase-Based Rehabilitation
- Acute Phase (0–2 weeks): Cryotherapy, compression, and elevation to manage swelling.
- Subacute Phase (2–6 weeks): Passive motion bikes and aquatic therapy.
- Strengthening Phase (6–12 weeks): Resistance bands and step-ups.
- Functional Phase (3–6 months): Plyometrics and sport-specific drills.
Pain Management
- Multimodal Approach: Combine acetaminophen, gabapentin, and ice therapy.
- Avoid Opioids: Limited to 3–7 days due to dependency risks.

7. Non-Surgical Alternatives
Physical Therapy Protocols
- Neuromuscular Training: Improves proprioception in ACL-deficient knees.
- Eccentric Exercises: Lengthens muscles under tension to strengthen tendons.
Injections
- Hyaluronic Acid: Viscosupplementation for mild OA (6-month efficacy).
- Corticosteroids: Short-term relief but limited to 3–4 injections/year.
Lifestyle Modifications
- Weight Loss: A 10% reduction cuts knee stress by 20–30%.
- Bracing: Unloader braces for OA redistribute joint forces.
8. Cost of Knee Surgery
Global Cost Comparison
U.S.: TKR averages
- 30,000 USD
- 30,000–50,000 USD.
India:
- 7,000 Rs.
- 7,000–10,000 Rs. with similar quality outcomes.
Germany:
- 15,000 EUR
- 15,000–20,000 EUR, covered by public insurance.
Insurance Navigation
- Prior Authorization: Required for most procedures; submit MRI/X-ray evidence.
- Appeals Process: 30% of initial denials are overturned with physician letters.
9. FAQs
Q: How long do knee implants last?
A: 90% last 15–20 years; ceramic and oxidized zirconium models may exceed 25 years.
Q: Can I kneel after knee replacement?
A: Yes, but 50% of patients report discomfort; use padded cushions.
Q: What’s the success rate of meniscus repair?
A: 70–80% if done within 6 weeks of injury and in vascular zones.
Conclusion
The future of knee surgery lies in personalized care—combining robotics, biologics, and patient-specific rehabilitation. By partnering with a board-certified orthopedic surgeon, you can tailor a plan that aligns with your activity goals, health status, and financial capacity. Explore non-surgical options early, but don’t delay surgery if it promises lasting relief. For further insights, read our guides on Preventing Joint Degeneration or Nutrition for Bone Health.
